SMART SOURCING
OPERATIONS CONSULTING


 |
 |
In order to create an IDS focused on evidence based medicine and population health management, the any PPS will require clear communication and integration among all providers throughout the PPS network.
There will need to be a common platform permitting complete, accurate real time communications between and among all inpatient, subacute, skilled nursing, clinic, behavioral health, post-acute, long term care, and community-based organizations to transition from an inpatient-centered to a community-based care delivery system.
As highlighted by Julie A. Jacobs, MPH; Ellen Jones, PhD; Barbara A. Gabella, MSPH; Bonnie Spring, PhD; Ross C. Brownson, PhD in their 2012 paper titled “Tools for Implementing an Evidence-Based Approach in Public Health Practice” (http://www.cdc.gov/pcd/issues/2012/11_0324.htm), among the key elements of Evidence Based Public Health are the following:
These key elements further reinforce the need for clear communication and integration between and among all components of the provider network within and throughout any PPS.
This will help transform the PPS from a disaggregated group of previously non-communicative providers into an IDS delivering best evidence based, high quality care at the right time and place at an affordable cost.
Meryl Bloomrosen and Don E Detmer refer to three stages of technology implementation which may also be applicable to the successful functioning of all Performing Provider Systems:
The technology assets that will be required to permit all PPSs to achieve their performance objectives need to have the following characteristics. They will need to:
There are significant challenges to providing PPS wide technology assets outlined above. There are three principal issues from the technology and operations perspective as follows:
In addition to these, the PPS should ensure that the team assigned to build and manage these technology assets has prior experience in undertaking successfully such implementations.
BISIL has experience and expertise building end to end processes and solutions. These start with patient on-boarding, assessing patients’ health and stratifying them by risk, care planning, managing and coordinating care including referrals, and providing an integrated single view longitudinal record of patient care.
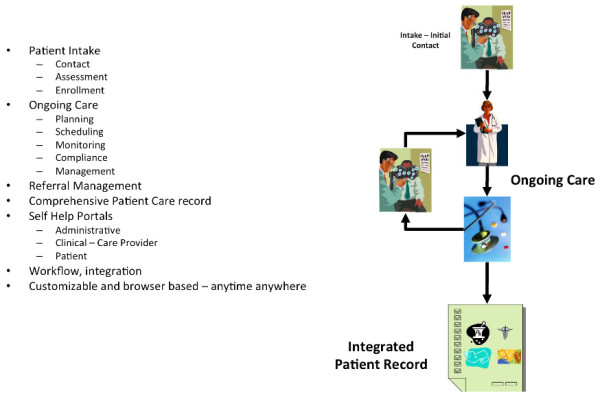
An example of the care planning process is shown in the schematic below. On the basis of the initial patient on-boarding, assessment and risk stratification, the care team formulates the care plan for the patient. The inputs into this care plan include working diagnoses, alternative treatment plans, ultimate care objectives and barriers to achieve them that are assessed during the initial on-boarding and stratification processes. This care plan then becomes a ‘living’ part of the patient care process and can be continuously adjusted and fine-tuned based on patients’ evolving needs.
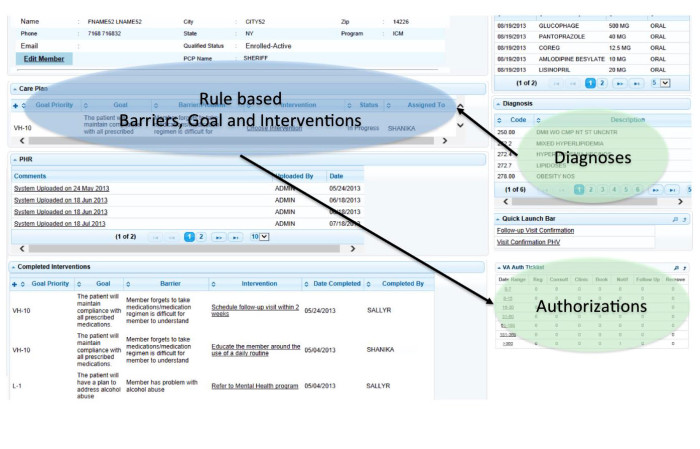
All the steps outlined above require data from all the participants in the PPS. As shown in the schematic, alongside the BISIL solution framework architecture are the necessary components to integrate data from different recorded sources, normalizing and standardizing all these into a common data set structure, Achieving that creates a meaningful data warehouse.

The data may be integrated via a Master Patient Index and other related references, so that data from different sources can be put together in a context readily available for different uses.
BISIL’s project methodology includes an evaluation of the software assets available within our clients compared to relevant software assets within BISIL, based on their relative capabilities (either separately or in various combinations) to achieve desired outcomes. Once the project specifications have been finalized, BISIL will use an agile approach that includes:
BISIL uses “Enj” – Business Process Management Suite built on open world technologies. While Enj comprises various components that may be productively used in the configuration of the desired solution, Enj easily integrates with any other system that provides access to its data repository.
Useful especially in healthcare implementation, BISIL has successfully worked with multiple electronic health information technologies (eHITs) to marshal data across the landscape and present actionable interfaces that comply with the requirements of a fully functional and integrated system. BISIL achieves this with minimal invasiveness as possible to avoid disturbing “business as usual” needs while the underlying system transformation progresses.
BISIL’s implementation plan is tailored to the specific priorities of a PPS network providing for an iterative approach to developing and deploying it as an IDS promoting evidence based medical practices and population health management. While the overall implementation plan, deliverables and expected system outcomes will be agreed upon and documented upfront, implementation can be staged in multiple ways such as:
Depending upon specific requirements, BISIL may go in for a big-bang one-time implementation, or a comparatively lower invasive approach, without affecting the ability of the PPS to meet all time-sensitive requirements to obtain maximum reimbursement through the DSRIP Program.
| Project 2ai Requirement | BISIL’s contribution | |
| 1 | The IDS should include all medical, behavioral, post-acute, long-term care, and community-based service providers within the PPS network; additionally, the IDS structure must include payers and social service organizations, as necessary, to support its strategy. | Our system will take care of integrating with all underlying systems subject to normal data transfer protocols with very low invasiveness |
| 2. | Utilize partnering HH and ACO population health management systems and capabilities to implement the strategy towards evolving into an IDS | Utilizing our BPM platform we will be able to work with any Population Health system with standard protocols |
| 3 | Ensure that all PPS safety net providers are actively sharing EHR systems with local health information exchange/RHIO/SHIN-NY and sharing health information among clinical partners, including direct exchange (secure messaging), alerts and patient record look up, by the end of Demonstration Year (DY) 3. | BISIL’s care coordination/ management system will provide for secure messaging, alerts and patient record look-ups including with mobile interfaces |
| 4 | Ensure that EHR systems used by participating safety net providers must meet Meaningful Use and PCMH Level 3 standards by the end of Demonstration Year (DY) 3. | These are specific EHR Meaningful Use and Patient-Centered Medical Home requirements which every PPS will need to achieve by December, 2017. |
| 5 | Perform population health management by actively using EHRs and other IT platforms, including use of targeted patient registries, for all participating safety net providers. | –to fill— along with WISE capabilities for analytics Much of this will be fulfilled by a Population Health Management IT firm, but WISE may play an important health data analytics role in transforming the data produced by these PHM practices into actionable information and knowledge-based learning systems. |
| 6 | Achieve 2014 Level 3 PCMH primary care certification for all participating PCPs, expand access to primary care providers, and meet EHR Meaningful Use standards by the end of Demonstration Year (DY) 3. | This is similar to #4 above, and something which the provider partners within every PPS will need to achieve by the end of 2017. |
| 7 | Re-enforce the transition towards value-based payment reform by aligning provider compensation to patient outcomes. | BISIL’s system will incorporate the road map and infrastructure for providing value based compensation based on agreed clinical outcomes and responsibility assignment |
| 8 | Engage patients in the integrated delivery system through outreach and navigation activities, leveraging community health workers, peers, and culturally competent community-based organizations, as appropriate. | BISIL will facilitate this patient engagement both on line and through mobile interfaces (to the extent that these are also available to Medicaid beneficiaries) |
Watson Institute for Systems Excellence (or WISE) is an institute of advanced studies at Binghamton University, a group that has been working with industry on applied research for over 25 years now (since May 1989).
One of the fastest areas of growth within the group is healthcare systems engineering/operations management/analytics/data science. WISE’s vision is to become “an internationally renowned multi-faceted customer focused organization that assists industry in a cost-competitive manner while concurrently enhancing competitiveness of industry”. Furthermore, WISE’s mission is “to create and sustain a value driven relationship between industry sponsors and academia”.
Today, WISE works with about 25+ sponsors, located all over the U.S., from Cambridge (Massachusetts) to San Jose (California). The work with our customers (industries) is carried out in a collaborative mode, on research endeavors that are of interest to them. Our customers include industry leaders such as IBM, Google, Mount Sinai Health System, Cooper Health, Analog Devices, Sanmina-SCI, Innovation Associates, Montefiore Medical Center, Smart Modular Technologies, Bennett Distribution Services, etc. Today, our team includes over 75 graduate students (both at the MS and PhD levels) along with faculty members and staff. Over the past two and a half decades, we have graduated over 450 graduate students (MS and PhD).
On the international front, WISE has recently completed a research project in the Philippines (with one WISE graduate research associate being placed in Manila). We continue to work with international sponsors such as Samsung and LG (Life’s Good). We also have existing research efforts in India and China, to name a few examples. The applied research work that we conduct with industry every year is worth $2.5-3.0 million (with more than 80% of this work being done outside the Binghamton area).
The WISE graduate students (MS and PhD) usually work at our sponsor’s (customer’s) facility, and are co-directed by both a mentor from the sponsoring entity (e.g., a hospital system) and from the university (research scientists and faculty members).
Our students are at the graduate level, pursuing either their MS or PhD. If our students are working at a location that is not in the immediate geographic region around Binghamton, they can take classes, if needed, through EngiNet (our distance learning mechanism).
Healthcare systems engineering and healthcare operations/systems management/data science represent areas of significant expertise and knowledge for our research group, both in terms of research and education related activities. WISE has established a national reputation in the healthcare systems area since 2001/2002 through collaborative partnerships on a wide spectrum of projects with multiple U.S. hospital systems on site.
These partnerships focus on applied research projects that can be broadly classified under:
(a) Workflow and process re-design
(b) Productivity assessment and capacity planning
(c) Strategic planning and future-state analysis
(d) Lean six sigma training and implementation
(e) Integrated clinical environment modeling and analytics
(f) Digital human modeling for ergonomic assessment
Examples of this research include optimizing the use of OR suites, outpatient scheduling, pre-admission testing, reducing patient turnaround time in emergency rooms, reducing turnaround time of medications/lab results, optimizing the deployment of mobile intensive care units, prediction of hospital readmissions/falls/pressure ulcers, statistical modeling and simulation, staffing models development, as well as ergonomic study and evaluation of patient handling activities/procedures, just to name a few.
Our portfolio of projects is very broad in nature and covers basic and applied research.
These efforts have been supported through partnerships with several U.S. hospital systems and healthcare organizations, including United Health Services (Binghamton, NY), Virtua Health (Marlton, NJ), the Mayo Clinic (Rochester, MN), Mount Sinai Health System (Manhattan, NY), Montefiore Medical Center and the Care Management Organization (Yonkers, NY), LiveOnNY (Manhattan, NY), Upstate University Hospital (Syracuse, NY), the Veterans Health Administration (Boston, MA), and Cooper Health (Camden, NJ).
In addition to these efforts with various hospital systems, WISE has developed a Healthcare-based Lean Six Sigma training program at both the Green Belt (40 hours of instruction) and Yellow Belt (20 hours of instruction) levels.
Unlike traditional lean six sigma training (involving significant manufacturing emphasis), our program is completely healthcare-focused, which makes it easy for healthcare professionals of various backgrounds (e.g., doctors, nurses, pharmacists) to understand. In fact, healthcare professionals/clinicians of virtually any background can participate in those programs. Thus far, our group has been able to successfully deliver this training (at both levels – Green and Yellow) to two hospital systems since 2011.
WISE will complement the efforts in building the IDS by developing advanced analytics. Four case studies illustrate that readmissions per se were not the sole focus of top-performing hospitals (low readmission rates) in the U.S.
Instead, they set the goal of achieving superior clinical and care-quality performance (Silow-carroll et al., 2011). Therefore, WISE is proposing a systems engineering approach to manage population health with a focus on performance improvement using a rich set of techniques from the discipline of industrial and systems engineering.
In particular, in order to achieve population health management, a systems engineering approach needs be adopted by taking a holistic view of healthcare-related activities and outcomes at the community level. The rich skill sets available to WISE make this approach feasible and implementable.
Besides expertise and experiences with analytics to be performed towards achieving DSRIP goals as mentioned in the next section, WISE has a very significant level of knowledge and extensive experience of applying lean six sigma techniques to healthcare delivery systems.
For instance, WISE has drawn many process maps, value stream maps, SIPOC (Suppliers, Inputs, Process, Outputs, and Customers) maps, swim-lane diagrams, fish-born diagrams, as well as applying DMAIC (Define, Measure, Analyze, Improve, Control) framework and root-cause analysis to understand and then improve the process.
The WISE has expertise in formulating and solving optimization problems with tools such as linear programming, nonlinear programming, heuristics and meta-heuristics (e.g., genetic algorithm, Tabu search, simulated annealing, and so on). Some examples of optimization problems include determining the optimal level of staffing, and identifying optimal pricing strategies by Health Information Exchanges. After collecting necessary data, WISE typically performs statistical analyses to describe and characterize the data, and test various hypotheses.
WISE also has expertise and experience in developing various prediction models for healthcare delivery, including breast cancer diagnosis (highest accuracy reported in the literature), Erythemato-Squamous cell cancer disease classification, 30-day mortality for four diagnosis related groups (DRGs), daily and hourly patient arrivals to emergency departments (EDs) and walk-in clinics, admissions and discharges to inpatient units, and the projection of future healthcare expenditures.
The modeling methods include time series models (e.g., autoregressive integrated moving average, ARIMA), logistic regression, decision tree, random forest, support vector machine (SVM), artificial neural networks, hybrid models (e.g., particle swarm optimization based SVM) among others.
Several significant implications could result from these prediction models. With improved diagnosis accuracy, clinical outcomes of the target population are likely to improve with possibly significant reduction in waste of expensive healthcare resources. With more accurate forecast of demand (to EDs, walk-in clinics, inpatient units, etc.), expensive healthcare resources could be better aligned with uncertain demand leading to improvement in resource utilization and patient/staff satisfaction.
Proactively identifying patients with probable future high healthcare costs could allow targeted and effective interventions to reduce those costs, improving the financial status of those paying for care while improving the health status of the entire community. Improving performance at multiple fronts would provide strong supports for effective population health management.
In addition, WISE has extensive experience in building simulation models and conducting simulation-based analyses for a wide range of processes in healthcare delivery.
For instance, WISE successfully developed a simulation model for the split flow process in the emergency department. Furthermore, WISE conducted “what-if” experiments statistically comparing key performance metrics between a baseline and alternative scenarios. WISE has experience in scheduling patients and healthcare resources in a cost-efficient manner.
Overbooking and overlapping scheduling strategies have been experimented and evaluated with simulation models. Moreover, scheduling a number of medical tests simultaneously is studied with multi-objective optimization, which is solved with various meta-heuristics (optimization techniques) and constraint programming.
Some of the improvements observed include increase in patient throughput, reduction in patient wait time and turnaround time (and thus improvement in patient/provider satisfaction), significant cost-saving from optimal staffing and streamlined processes, data-driven changes in facility layout, etc.
WISE is experienced and has needed resources to perform data mining using machine learning techniques in order to achieve DSRIP goals. WISE will develop a data-driven framework to identify patient groups at high risk for readmission at four different levels including disease-specific, population, institutional, and system levels.
Ahmad, F. S., Metlay, J. P., Barg, F. K., Henderson, R. R., & Werner, R. M. (2013). Identifying hospital organizational strategies to reduce readmissions. American Journal of Medical Quality, 28(4), 278-285.
Silow-Carroll, S., Edwards, J. N., & Lashbrook, A. (2011). Reducing hospital readmissions: lessons from top-performing hospitals [Internet]. New York (NY): Commonwealth Fund [cited October 6, 2015].
Available from: http://www.commonwealthfund.org/~/media/files/ publications/case-study/2011/apr/1473_silowcarroll_readmissions_synthesis_web_version.pdf
Copyright 2014 © Transnational Business Solutions LLC | All rights reserved. Disclaimer | Privacy Policy